The shoulder is the most mobile joint in the human body, which makes it prone to instability. These instabilities can result from soft tissue injuries or bony defects, often occurring after dislocation or chronic strain. Accurate diagnostics are crucial to identify the underlying pathology and determine the optimal treatment strategy.
Classification and Basics of Shoulder Instability
Shoulder instabilities can arise due to trauma, overuse, or anatomical peculiarities. A proven system for classification is the FEDS classification system (Frequency, Etiology, Direction, Severity). It considers the frequency of instability episodes (single, occasional, frequent), their cause (traumatic or atraumatic), the direction of instability (anterior, posterior, or inferior), and the severity (subluxation or complete dislocation). This system enables quick and effective categorization of symptoms, which is essential for further diagnostics and treatment planning.
| Frequency | Episodes per year single: 1 episode occasional: 2-5 episodes frequent: > 5 episodes |
| Etiology | traumatic atraumatic |
| Direction | anterior inferior posterior |
| Severity | subluxation dislocation |
Imaging: The Key to Diagnostics
Choosing the right imaging modality is essential for assessing shoulder instabilities!
A simple X-ray is insufficient for diagnosing pathologies resulting from dislocation or causing chronic instability.
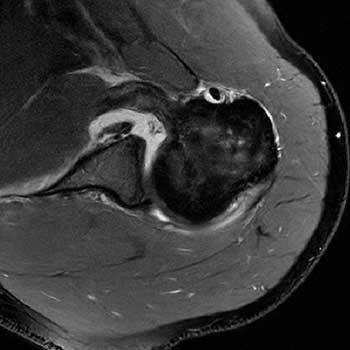
Magnetic Resonance Imaging (MRI) provides excellent visualization of soft tissue injuries and is considered the gold standard.
Since both soft tissue injuries and bony lesions can cause instability, a Computed Tomography (CT) scan is often recommended. CT scans with 3D reconstructions are the standard for assessing bony defects. The 3D reconstruction allows visualization of the glenoid surface by subtracting the humeral head, enabling detection of even minor bone loss. It also provides optimal imaging and measurement of Hill-Sachs lesions.

Newer MRI techniques with 3D sequences offer promising alternatives, especially for patients who should avoid radiation exposure from CT scans.
Additionally, ultrasound can be used for dynamic tests and assessing the rotator cuff.
Soft Tissue Injuries as a Cause of Shoulder Instability
The soft tissues of the shoulder include the labrum, capsule, glenohumeral ligaments, and rotator cuff. Injuries to these structures often lead to instability, particularly after trauma.
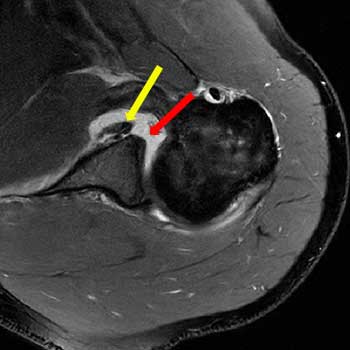
Labral and capsular injuries are common findings in patients with anterior instability. A typical injury is the Bankart lesion, where the anteroinferior labrum tears away from the glenoid. This lesion often occurs after an initial dislocation.
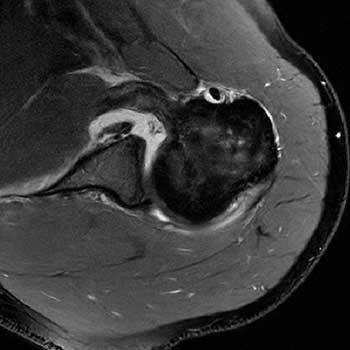
Another common pathology is the SLAP lesion (Superior Labrum Anterior to Posterior), particularly seen in overhead athletes like volleyball or tennis players. Diagnosis is primarily achieved via contrast-enhanced MRI, providing high-resolution images of soft tissue structures. In uncertain cases or for surgical planning, diagnostic arthroscopy may be necessary.
Dynamic stability disorders often affect the rotator cuff. These muscles are crucial for active stabilization of the joint. Chronic rotator cuff damage, more common in older patients, can also contribute to instability.
Bony Lesions: Types and Clinical Significance
Bony defects caused by dislocations or chronic strain are a common cause of recurrent shoulder instability. Glenoid and humeral head defects are particularly relevant.
Glenoid defects occur due to anteroinferior dislocations where part of the glenoid is eroded. Such defects alter the shape of the socket, reducing its ability to center the humeral head. Studies show that defects greater than 20% of the glenoid width significantly increase recurrence rates after soft tissue repair alone. CT with 3D reconstruction is the gold standard for accurate assessment. The Glenoid Track concept helps assess the risk of recurrent dislocation by evaluating whether the humeral head remains within the load-bearing zone of the glenoid.
Another common problem is the Hill-Sachs lesion, a dent in the posterolateral humeral head caused by dislocation. These lesions are particularly problematic when combined with a glenoid defect, as they further decrease joint stability. Accurate assessment is also achieved through CT or MRI. Dynamic evaluation during arthroscopy can identify "engaging" lesions, where the defect locks into the glenoid during arm movement.
Modern Diagnostic Concepts: On- and Off-Track Lesions
A key advancement in diagnosing shoulder instabilities is the On- and Off-Track concept. This concept evaluates whether a Hill-Sachs lesion lies within (on-track) or outside (off-track) the load-bearing area of the glenoid. Off-track lesions have an increased risk of recurrent instability and often require specific surgical treatment.
Conclusion
Diagnosing shoulder instabilities requires precise clinical and imaging evaluations to accurately characterize soft tissue and bony lesions. Concepts such as the Glenoid Track model and On- and Off-Track classification enable better predictions of recurrence risk and optimized treatment planning. With modern diagnostic approaches, tailored treatments can be planned to restore the long-term function and stability of the shoulder.
```









